RxFiles Academic Detailing
www.RxFiles.ca
RxFiles Academic Detailing
© www.RxFiles.ca
Page 1 of 2
Opioid Tapering Template
For use when a decision is made to reduce or discontinue an opioid in chronic non-cancer pain (CNCP).
General approach considerations:
1. In discussion with the patient, set a reasonable start date for the taper.
2. Gradual tapers can often be completed in the range of 1 to 6 months. However, some may benefit from a longer time
frame of 12-24 months. Initial daily dose reductions in the range of 5-10% every 2-4 weeks are reasonable.
1
Once a dose of
approximately 1/3 of the original dose is reached, smaller dose reductions (e.g. 5% every 4-8 weeks) may be more suitable
for some & more likely to result in a successful taper.
1
More rapid tapers are possible and sometimes desired. In such cases,
use of an opioid withdrawal scale (e.g. COWS) & corresponding withdrawal protocols may be recommended, allowing for
successful withdrawal within 1-2 weeks. (See links
2-4
)
3. Long-acting formulations that offer smaller dose increments are useful for more gradual tapers once in the lower end of
the dosage range. {Examples: morphine long-acting: M-ESLON 10mg cap
q12h
, KADIAN 10mg cap
q24h
.}
4. Consider daily dispensing of opioids or blister packs for those at high risk of overdose or aberrancy use.
5. Determine if the goal of dose reduction is reasonable (e.g. opioids have offered some benefit) or if complete
discontinuation is more suitable (e.g. opioid trial has been highly problematic/non-helpful or there is a concern regarding
opioid induced hyperalgesia).
6. If goal is to reduce dose, option to taper further & more gradually may be entertained at a later point. Tapering plan
may be held/reassessed at any point if pain/function deteriorate or withdrawal symptoms persist for 1 month or more.
However, the “hold off on further taper & plan to reassess/restart taper” conversation should have a designated
endpoint & be one conversation, not two!
7. Encourage functional goal setting & efforts to enhance non-drug approaches in management plan.
8. Optimize other pain management (e.g. Is something needed for neuropathic pain such as nortriptyline, gabapentin or pregabalin).
9. Anticipate likely and possible withdrawal effects & have a management plan in place. (See Pg 2 & Withdrawal Rx)
10. Given the complexities in some cases, discussion with experienced colleagues and an interdisciplinary approach will
help optimize management. Continue to use “best practice” tools (e.g. Opioid Manager, UDS).
11. Strongly caution patients that a) they have lost their tolerance to opioids after as little as a week or two of abstinence, &
b) they are at risk for overdose if they relapse/resume their original dose. OTC:
Consider a Take Home Naloxone Kit !
Timeline for discontinuation or reaching a taper “target dose”
Current dose ______________________________________________________
Proposed target dose _______________________________________________
Timeline (in weeks or months) __________________________ weeks months
Allow for gradual q3 day, weekly, bi-weekly or monthly dose reductions. Reassess as necessary.
In general, the longer the duration of previous opioid therapy, the more time should be allotted for tapering. Rate of
tapering should often be even more gradual as total daily dose reaches lower end of range (e.g. 120 mg Morphine/day)
See page 2 for customizable Tapering Template, or go online for customizable Opioid Withdrawal Prescription.
Name: __________________________________________ Date: ________________
Address: ___________________________________________________________________
(May switch/rotate to 50-75% equivalent morphine dose of an alternate opioid.)
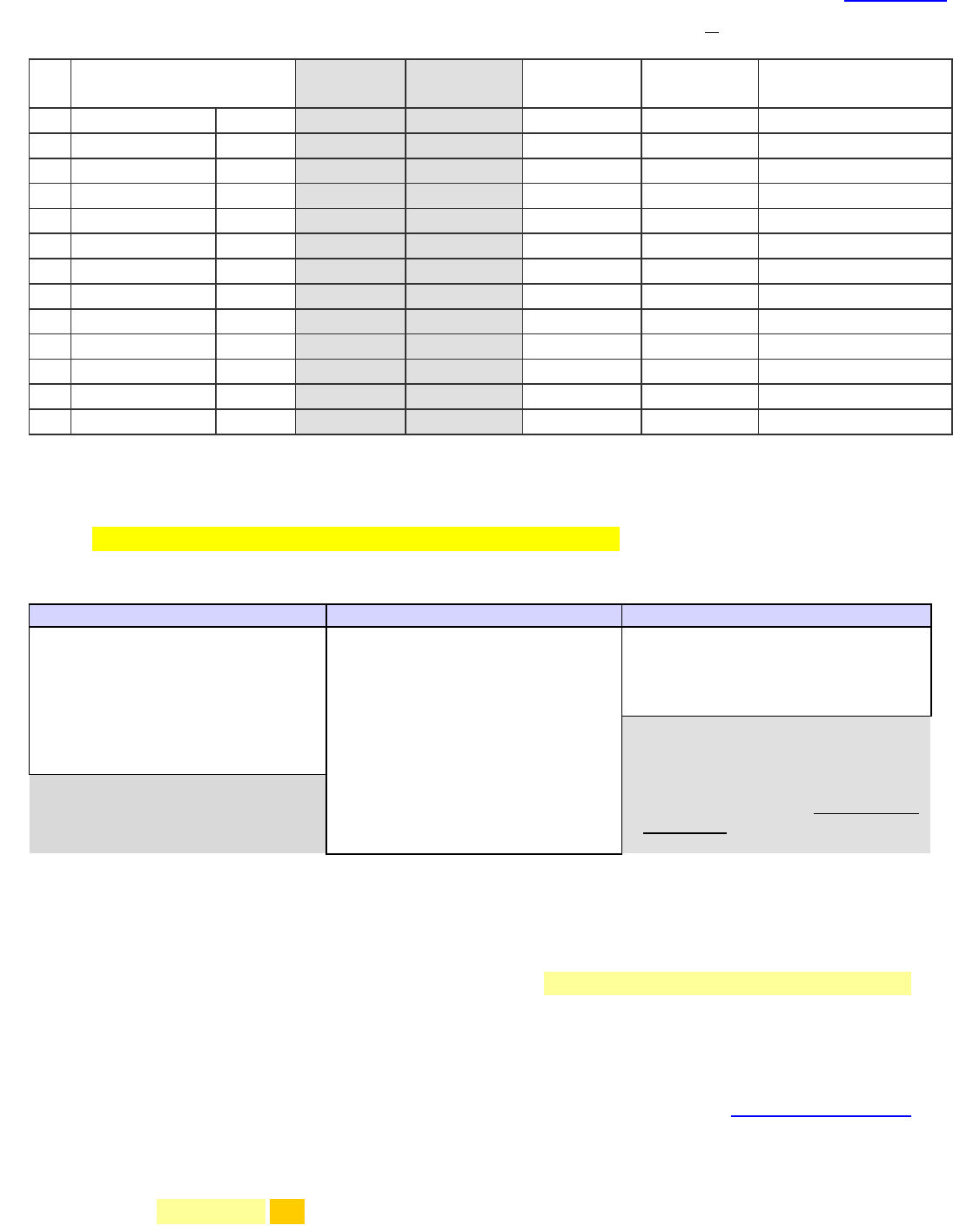
A) Tapering Schedule*: Drug _____________________________
Reduced dose accounts for incomplete cross tolerance. See Opioid Manager Switching Tool.
Dates (# wks)
AM Dose**
PM Dose
Other
Total
Dose/Day
Quantities Needed
0.
Current Regimen
-
$
mg
mg
mg
1.
Start Date!
x wk
mg
mg
mg
2.
x wk
mg
mg
mg
3.
x wk
mg
mg
mg
4.
x wk
mg
mg
mg
5.
x wk
mg
mg
mg
6.
x wk
mg
mg
mg
7.
x wk
mg
mg
mg
8.
x wk
mg
mg
mg
9.
x wk
mg
mg
mg
10.
x wk
mg
mg
mg
11.
x wk
mg
mg
mg
*template may be adjusted based on patient’s progress; decisions on further tapering, etc. Last 20-30 mg may require more time.
**if once daily formulation (eg. morphine SR KADIAN) record dose in respective AM or PM column & “0” in other.
$
individualize duration! May begin by reducing dose q2-4 weeks and then q4-8 weeks once 1/3 of the dose is reached.
B) Opioid withdrawal symptoms:
- Many of these symptoms may not be seen with a gradual taper!
- Physical withdrawal symptoms generally resolve by 5-10 days following opioid dose reduction/cessation.
- Psychological withdrawal symptoms (dysphoria, insomnia), if seen, may take longer (months) to resolve.
Early symptoms may include:
Late symptoms may include:
Prolonged symptoms may include:
- anxiety and restlessness
- sweating
- rapid short respirations
- runny nose, tearing eyes (minor)
- dilated reactive pupils
- brief
in pain (usually few
days)
- runny nose, tearing eyes
- rapid breathing, yawning
- tremor, diffuse muscle
spasms/aches
- pilo-erection (goose bumps)
- nausea and vomiting; diarrhea
- abdominal pain
- fever, chills
- white blood cells (if sudden
withdrawal)
- irritability, fatigue; hormonal
related
- bradycardia (slower heart rate)
- decreased body temperature
Some people with chronic pain will
find that symptoms such as fatigue
& general well-being are improved
over time with tapering of the
opioid. In such cases, gradual gains
in function will be possible &
should be explored.
Early = hours to days
Late = days to weeks
Prolonged = weeks to ~6 months
C) NSAID (e.g. naproxen
250-375mg twice daily
or ibuprofen
400-600mg four times daily
): useful for pain & withdrawal aches/pains.
D) Laxative: continue initially; with time, or if diarrhea emerges, reduce, hold & eventually stop laxative
(See Q&A)
5
E) Management of other side effects:
1. Clonidine 0.1mg twice daily PRN (up to 4 times daily) may be prescribed for general relief/prevention of physical
withdrawal sxs. (Caution if SBP <100, orthostasis, or HR <60); Some patients may not require if gradual taper. May use SOWS
(patient administered scale) for monitoring (e.g. score 10-20 take clonidine) see Pg 9. [Cochrane review documented use for
7-14 days up to 30 days,
6
but some may need longer]. If used regularly, taper, over ~7-10d, to stop.
2. Acetaminophen (650-1000mg every 6 hours as needed) may be used for aches, pains, flu-like symptoms.
3. Loperamide may be used as necessary for diarrhea; however, may not need with gradual taper.
4. Non-drug & “sleep hygiene” measures should be employed
(e.g. U of R pain course www.onlinetherapyuser.ca/pain; regular
bedtime/wake-time; sleep restriction)
.
7-9
If additional tx required, short-term trazodone 25-50-100mg HS is an option.
5. Dimenhydrinate 50-100mg every 6 hours as needed for nausea/vomiting
[Alternatives: prochlorperazine 5-10mg q6h, haloperidol 0.5-1mg q12h]
6. Other
7. Remember tolerance to previous dose of opioid is lost after 1-2 weeks!
Consider Naloxone Kit OTC for risk of overdose!
Physician: ____________________________
Page 2 of 2
Opioid Tapering
Template
© www.RxFiles.ca
Extras, Links & References © www.RxFiles.ca
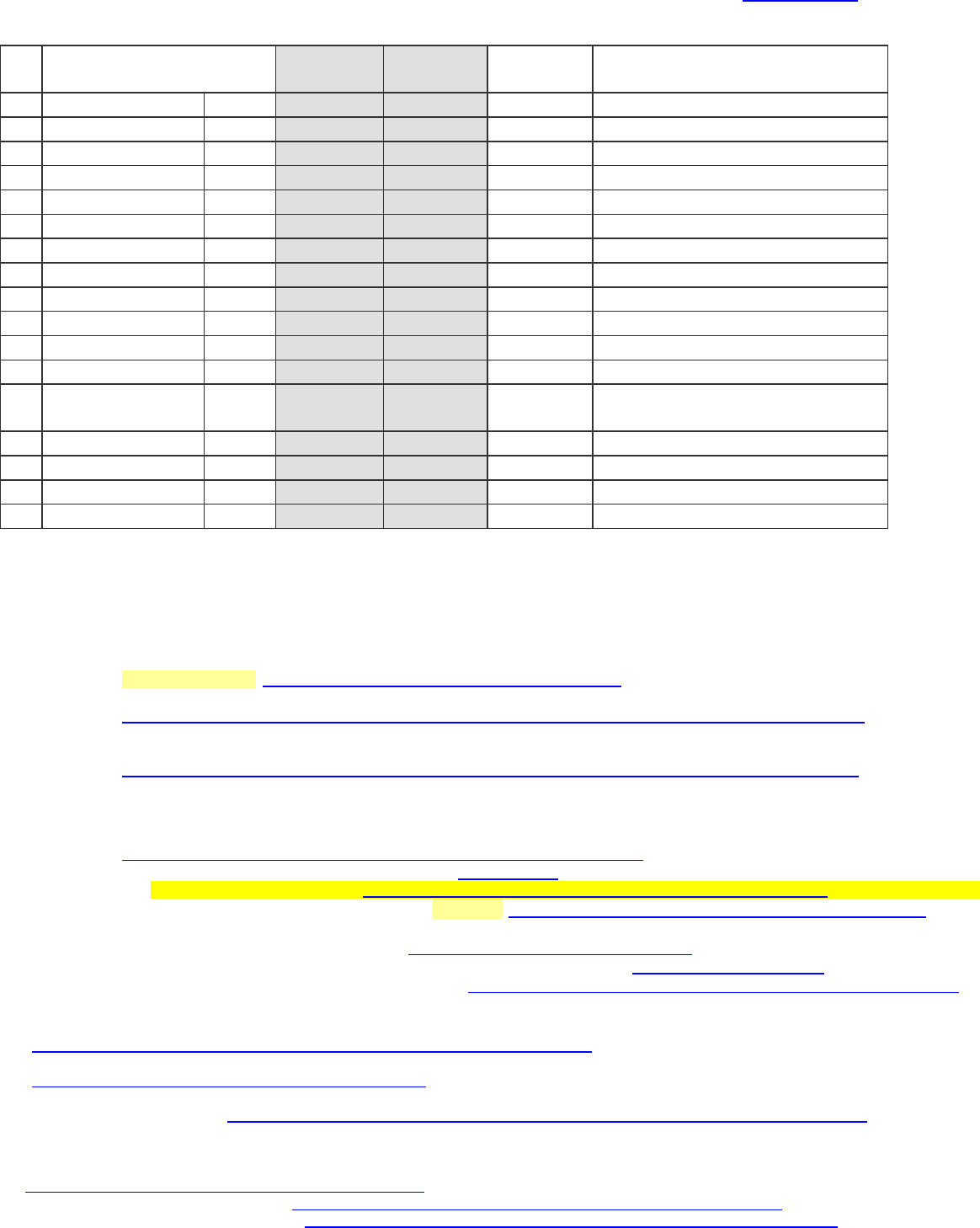
A) Sample Slow Tapering Schedule*: Drug _____Morphine long acting_(MS CONTIN)
Dates (# wks)
AM Dose**
PM Dose
Total
Dose/Day
Quantities Needed
0.
Current
-
245mg
245mg
490 mg
1.
X2 wk
230 mg
230 mg
460 mg
(4x100mg) + (2x30mg) x14d
2.
X2 wk
215 mg
215 mg
430 mg
3.
X2 wk
200 mg
200 mg
400 mg
4.
X2 wk
190 mg
190 mg
380 mg
5.
X4 wk
175 mg
175 mg
350 mg
6.
X4 wk
160 mg
160 mg
320 mg
7.
X4 wk
145 mg
145 mg
290 mg
8.
X4 wk
130 mg
130 mg
260 mg
9.
X4 wk
115 mg
115 mg
230 mg
10.
X8 wk
100 mg
100 mg
200 mg
11.
X8 wk
90 mg
90 mg
180 mg
12.
X8 wk
80 mg
80 mg
160 mg
Switch to M-ESLON, or
once daily KADIAN for smaller titrations
13.
X8 wk
140 mg
0 mg
140 mg
14.
X12 wk
120 mg
0 mg
120 mg
15.
16.
*this template may be adjusted based on patient’s progress; decisions on further tapering, etc.
**if once daily formulation (i.e. KADIAN) record dose in respective AM or PM column and “0” in other.
-----------------------------------
Additional information:
1
2017 C anadian Guideline for Opioids for Chronic Pain (May 2017) - Links
Link to Guideline Site: http://nationalpaincentre.mcmaster.ca/guidelines.html
Opioid Tapering- Information for Patients – English:
http://nationalpaincentre.mcmaster.ca/documents/Opioid%20Tapering%20Patient%20Information%20(english).pdf
Opioid Tapering- Information for Patients – French:
Sevrage des opioïdes : informations à l’intention des patients.
http://nationalpaincentre.mcmaster.ca/documents/Opioid%20Tapering%20Patient%20information%20FRENCH.pdf
Other
CAMH: Video discussion of issues around how to taper.
http://knowledgex.camh.net/videos/Pages/tapering_presopioids_selby2013.aspx
RxFiles: Opioid Taper Template & related materials at: www.RxFiles.ca
o Pain/Opioid Resource Links: http://www.rxfiles.ca/rxfiles/uploads/documents/RxFiles-Pain-and-Opioid-Resource-Links.pdf
o RxFiles Pain/Opioid Newsletter Part 1 – Fall 2017: http://www.rxfiles.ca/rxfiles/uploads/documents/Opioids-Pain-2017-Newsletter.pdf
TheWell (Centre for Effective Practice):
o Opioid Tapering Template (2018) at: https://thewellhealth.ca/opioidtaperingtool
o Opioid Manager tool to support the Canadian Opioids in CNCP guideline: https://thewellhealth.ca/pain
CDC - POCKET GUIDE: Tapering Opioids For Chronic Pain: https://www.cdc.gov/drugoverdose/pdf/clinical_pocket_guide_tapering-a.pdf
2
Clinical Opiate Withdrawal Scale (COWS).
https://www.drugabuse.gov/sites/default/files/files/ClinicalOpiateWithdrawalScale.pdf
3
Subjective Opiate Withdrawal Scale (SOWS).
http://www.bccsu.ca/wp-content/uploads/2017/08/SOWS.pdf
4
Butt P, McLeod M. Opioid withdrawal protocol, Saskatchewan.
5
Opioid Induced Constipation Q&A: http://www.rxfiles.ca/rxfiles/uploads/documents/members/Opioid-Induced-Constipation-QandA.pdf
6
Gowing L, Farrell MF, Ali R, White JM. Alpha2-adrenergic agonists for the management of opioid withdrawal. Cochrane Database Syst Rev. 2014 Mar
31;3:CD002024.
7
Merrigan JM, Buysse DJ, Bird JC, Livingston EH. JAMA patient page. Insomnia.JAMA. 2013 Feb 20;309(7):733. Accessed online 21 Oct, 2013 at
http://jama.jamanetwork.com/article.aspx?articleid=1653524 .
8
Sedative Patient Information Sheet (RxFiles) http://www.rxfiles.ca/rxfiles/uploads/documents/PSYC-Sedative-PtHdout.pdf
9
Chronic Insomnia in Older Adults (RxFiles Q&A) http://www.rxfiles.ca/rxfiles/uploads/documents/Insomnia-Older-Adults-QandA.pdf
